MSU researcher is studying, raising awareness about the role of sex in the efficacy of vaccines that make use of nanomedicine. If there's one take-home message for the general public about the coronavirus vaccines approved in the U.S., it's that they are remarkably effective.
But Michigan State University's Morteza Mahmoudi is raising awareness about an important subtlety: The vaccines developed by Moderna and Pfizer-BioNTech appear to work slightly better for men than for women.
How's that possible?
Both vaccines use tiny orbs, or nanoparticles, to deliver their active ingredients to cells in our immune systems. For years, Mahmoudi has been studying how and why nanomedicines -- therapies that use nanoparticles - can affect patients differently based on their sex and he believes this could be a factor with the vaccines.
The Johnson & Johnson vaccine has also drawn attention to sex differences because its rare blood-clotting side effect has affected predominantly women. The J&J vaccine, however, uses modified adenoviruses rather than nanoparticles to help teach our immune systems to fight off the coronavirus. That said, Mahmoudi has shown in earlier work that viruses can transfect the cells of men and women differently.
Now, he's focusing on the nanomedicine component. He's published three peer-reviewed papers calling attention to the role of sex in nanomedicine studies, both in general and as they relate to coronavirus vaccines.
"We need to monitor these sex differences and report them to the scientific community and the public," said Mahmoudi, an assistant professor in the Department of Radiology and the Precision Health Program. "It can be very helpful in developing future strategies and as we prepare for future threats."
To develop those future strategies, researchers must better understand what causes patients of different sex to respond differently to nanomedicines, Mahmoudi said. To that end, Mahmoudi is advocating for systemic changes in how nanoparticles are used and studied in medicine with an article published May 20 in the journal Nature Communications.
Role of gender in nanomedicine
In the article, he outlines four large challenges in researching the role of sex in nanomedicine performance along with strategies to mitigate them moving forward.
For example, researchers may not have sufficient resources to perform their studies in cells or other samples taken from men and women. Yet these researchers and others may still interpret their results as being equally applicable to all sexes. To prevent this from happening, Mahmoudi is calling for researchers to be more transparent and share sex-specific limitations of studies and conclusions.
"We need to be more careful about the science that gets out," Mahmoudi said. "We've witnessed that there has not been a robust consideration of sex in nanomedicine, but we need to consider sex because it is important."
Before the coronavirus pandemic, most of the research interest and funding in nanomedicine had been focused on its use in treating cancer. But nanomedicine's performance in this realm has been lackluster. Less than 15% of nanomedicines that have entered clinical trials made it through the final phase and none have proven to be better than the standard of care, Mahmoudi said.
In addition, he said, when nanomedicines are robustly studied in women, it's often because the therapies are being studied in diseases that mainly affect women, such as breast and ovarian cancers.

"Our analysis of the 41 completed clinical trial studies of therapeutic nanomedicine products revealed that 21 studies were stratified by sex because they concerned pathologies primarily found in females," Mahmoudi said. "Of the remaining 20 studies involving 851 males and 430 females, none provided sex-stratified results or indications."
Mahmoudi's team detailed these findings and more in an article published online on May 4 in the journal Advanced Drug Delivery Reviews.
Despite their shortcomings in cancer therapies, nanoparticles have been greatly effective in helping provide protection against the novel coronavirus. Yet there is still evidence that the vaccines work differently for men and women.
"On the one hand, the vaccines have been really good news for nanomedicine," Mahmoudi said. "But we didn't solve the problems that we saw with them in cancer treatments."
To be clear, the differences in vaccine efficacy are small, but they are measurable. In the case of the vaccine developed by the pharmaceutical company Moderna, clinical trials showed it was 95.4% effective at preventing COVID cases for men, compared with 93.1% for women. For the vaccine created by Pfizer and BioNTech, the numbers are 96.4% for men and 93.7% for women.
Both vaccines use nanoparticles based on lipids, which are fatty molecules that form tiny spheres in water, kind of like bubbles. The pharma companies then pack these tiny lipid-based particles with the vaccines' active ingredients and essentially use the nanoparticles as delivery vehicles to ship the vaccines' payloads to our immune cells.
Working with researchers at Sapienza University of Rome, Mahmoudi designed an experiment to test whether lipid-based nanoparticles could be a reason behind the difference in vaccine efficacy for men and women. The team published its results on May 13 in the journal Molecular Pharmacology.
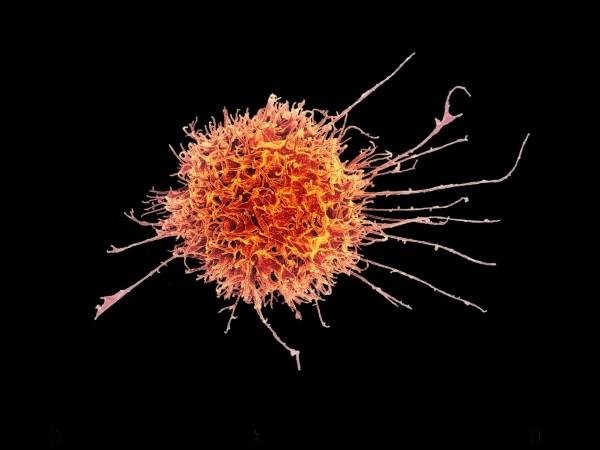
The team added lipid-based nanoparticles with similarities to those used in the vaccines to blood samples taken from 18 patients, eight men and 10 women. The researchers then observed how well or how poorly immune cells within the blood adsorbed those nanoparticles. The team found a significant difference between men and women for one cell type called natural killer cells.
"These cells are responsible for finding other infected cells -- cells that are producing the virus -- and they can kill them," said Mahmoudi. "What we found is that natural killer cells respond to lipid-based nanoparticles in a sex-specific manner."
Namely, natural killer cells from female donors took up fewer nanoparticles than natural killer cells from men. Based on this model system, then, it is plausible that the immune systems of men and women would respond differently to the vaccine.
But Mahmoudi and his colleagues also showed that the difference could be eliminated by first putting the nanoparticles in a donor's plasma, the cell-free portion of their blood sample. Mahmoudi believes this because proteins in the plasma can bind to the lipid-based nanoparticles, giving the nanoparticle a biological coating or corona.
"I think of the corona as acting like a new passport for nanoparticles, it tells the cells how to respond to nanoparticles," he said.
What this suggests, then, is that if there are differences in the vaccines' performance based on a patient's sex, doctors and researchers should be able to do something about it. But they'll need more research and data to fully understand the cause of and remedies to these differences, Mahmoudi said. Thankfully, though, the data available to the community is growing every day.
"The clinical trials were performed with tens of thousands of patients. We know that the differences are there and that we need to monitor them," he said. "Now we have millions of people getting the vaccines. That's millions of data points. We need to go out there and get them."

















