It is common knowledge now that the COVID-19 leads to significant damage of lung tissues among the infected. While the SARS-CoV-2 virus is responsible for cell death, the body's erratic immune responses have also been known to worsen the harm caused to the lungs. Now, a new study has found that a particular subtype of immune cells called macrophages plays a vital role in the hyper-inflammatory immune response in the lungs of individuals infected with the novel coronavirus.
According to a new study by South Korean researchers, infiltrating macrophages—along with promoting viral clearance—caused injury to lung tissues. It was learnt that immunosuppressant drugs used to treat hyper-inflammatory responses known as 'cytokine storm' also affect the identified macrophages. The research was published in the journal Nature.
"This study is the first longitudinal study using sequentially obtained immune cells originating from SARS-CoV-2 infected lungs. The research describes the innate immune response to COVID-19 using single-cell transcriptome data and enhances our understanding of the two phases of inflammatory responses," said Dr. Su-Hyung Park, corresponding author of the study in a statement.
Important Innate Immune Cells
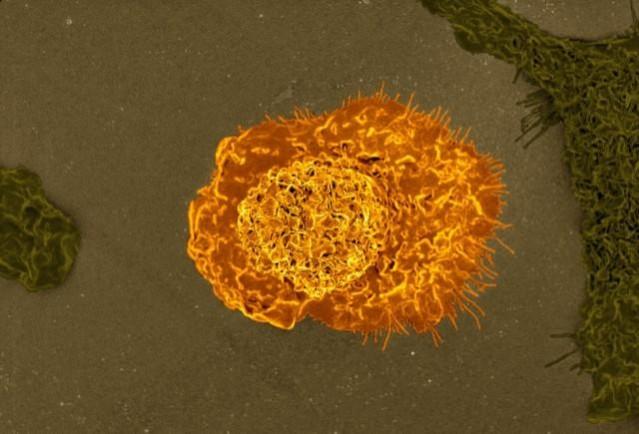
When a pathogen invades the body, a rapid response is triggered against it. This first line of defense is known as the innate immune system. Even in the case of COVID-19, innate immunity is activated against the SARS-CoV-2, driving immune cells present within the lungs into action. Cells known as macrophages form a major part of the innate immune system in the lungs. They detect, ingest (phagocytosis), and eliminate pathogens.
Macrophages are formed from white blood cells known as monocytes circulating in the blood, and the process is known as 'differentiation'. There are two types of macrophages—M1 and M2. These two categories comprise various subpopulations of macrophages. Depending on the proteins mediating the differentiation process, macrophages are differentiated into M1 (that promote inflammation) and M2 (that are anti-inflammatory).
For the study, which was a quantitative and qualitative evaluation of immune responses within the lungs, the team used a ferret model (Mustela putorius furo). Ferrets are susceptible to human respiratory infections and the histoanatomical features of their lungs provide an ideal platform for mimicking human infections. Therefore, the scientists exposed the ferrets to the SARS-CoV-2 virus and acquired infected lungs across a fixed time interval sequentially (two and five days).
Harming Lung Tissues
The examination of the immune microenvironment within the lungs revealed that there were notable changes in the characteristics and proportions of cells at two and five days post-infection. This was in comparison to uninfected control animals.
Next, based on gene signatures, 10 subpopulations of macrophages were observed over the course of infection. The analysis led to the identification of the key factor—infiltrating macrophages that originated from activated monocytes. Not only were they crucial for viral clearance but they played a role in damage to lung tissues as well.
It was also discovered that there were changes in the gene expression of the monocyte-derived infiltrating macrophages. Importantly, a specific macrophage subpopulation, DDX60+CHIT1(hi), that had undergone activation of inflammatory responses on account of the infection, was identified. Also, the differentiation process of these inflammatory macrophages was similar to the immune response within the lung tissues of patients suffering from severe COVID-19.
Effect of Immunosuppressants
It was also gleaned that the gene modules (a set of genes with similar expression functions) of these noted macrophages were downregulated by immuno-modulatory or immunosuppressive drugs such as corticosteroids. These agents are used to manage a hyper-inflammatory response known as 'cytokine storm' in COVID-19 patients.
Cytokines are signaling molecules that draw immune cells to the site of infection. However, in the case of some individuals with COVID-19, there is an erratic signaling response or a 'cytokine storm' that causes immune cells to attack healthy cells in the lungs.
Following the findings of the current research, the authors have commenced a follow-up study. The new investigation aims at identifying the dynamic changes of immune responses when immunosuppressive drugs are used to control cytokine storms. Talking about the study, Dr. Jeong Seok Lee, a corresponding author, expressed, "Our analysis will enhance the understanding of the early features of COVID-19 immunity and provide a scientific background for the more precise use of immunosuppressive agents targeting specific macrophage subtypes."





![Ultrahuman launches Ring PRO, free charging case with more than just power and Jade AI [details]](https://data1.ibtimes.co.in/en/full/829151/ultrahuman-launches-ring-pro-free-charging-case-more-just-power-jade-ai-details.png?w=220&h=138)











