3D printing is increasingly finding applications across numerous areas. Medicine is one such domain. From producing medical devices to human organs, the manufacturing technology has entrenched itself in the field. Now, using 3D printing, scientists have accomplished a pair of world firsts: printing human testicular cells and discovering encouraging signs of their sperm-producing abilities.
In a new multi-institutional study, researchers have successfully 3D printed testicular cells collected from a patient suffering from a severe form of male infertility. They found that these printed cells were able to grow into specialized cells that are essential for the production of sperm. These findings open new avenues into the treatment of male infertility that affects millions of men across the world.
"We're 3D printing these cells into a very specific structure that mimics human anatomy, which we think is our best shot at stimulating sperm production. If successful, this could open the door to new fertility treatments for couples who currently have no other options," said Dr. Ryan Flannigan, lead author of the study, in a statement.
Severe form of Male Infertility
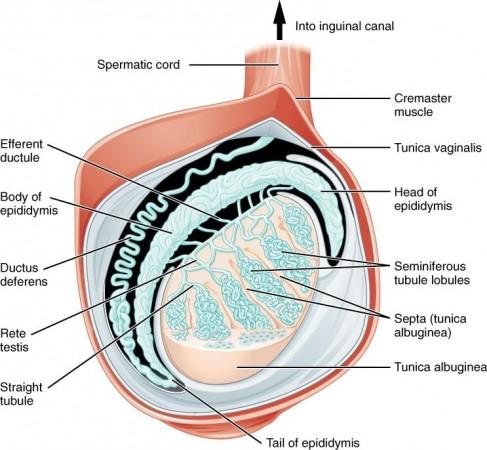
Tiny tubular structures are known as seminiferous tubules, that are found within the human testicles, produce sperm. In patients with non-obstructive azoospermia (NOA), the most extreme form of male infertility, no sperm can be detected in the ejaculate. This occurs as a result of a sharp decline in the production of sperm inside these tubes. Approximately 10-15 percent of infertile men are afflicted with this condition.
Though surgical intervention can provide some respite to patients with NOA by finding exceptionally rare sperm, Dr. Flannigan stated that the rate of success of the procedure is only around 50 percent. "Unfortunately, for the other half of these individuals, they don't have any options because we can't find sperm for them," he averred. It is this category of patients that the team hopes to aid.
Promising Signs
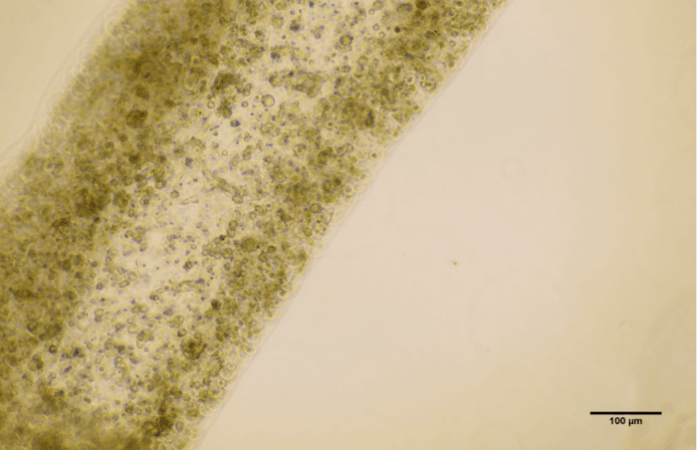
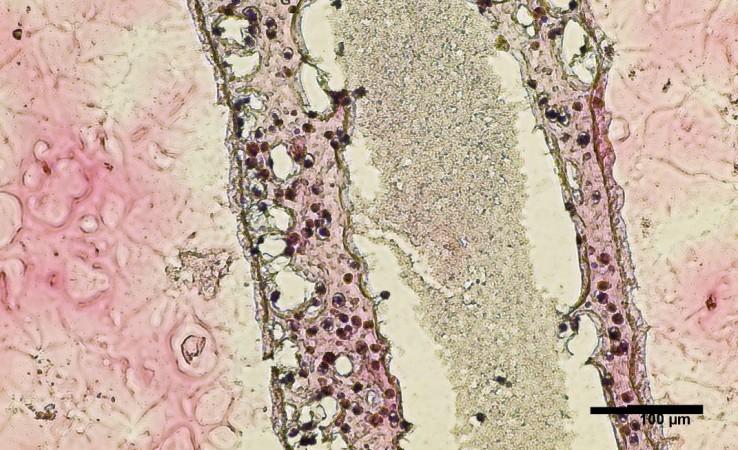
For the current study, the authors conducted a biopsy on the testicles of a patient struggling with NOA to obtain stem cells. These cells were cultured in vitro. Following this, the cells were 3D bioprinted (in a petri dish) into tubular structures that resembled seminiferous tubules.
Twelve days following the printing of the testicular cells, the researchers made an exciting discovery: the cells survived. In addition to surviving, they had also differentiated into several specialized cells that are closely involved in the production of sperm and were also exhibiting considerable improvement in the maintenance of spermatogonial stem cells.
The dual phenomenons serve as early indicators of sperm-producing abilities. "It's a huge milestone, seeing these cells survive and begin to differentiate. There's a long road ahead, but this makes our team very hopeful," noted Dr. Flannigan.
Hope for Infertile Men
Armed with the findings of the study, the scientists have begun attempting to 'coach' the 3D printed cells to produce sperm. In order to achieve this, the cells will be exposed to several growth factors and nutrients. Also, their structural arrangement will be fine-tuned in order to enable interaction between cells.
15% couples affected by infertility
According to Dr. Flannigan, around 15 percent of all couples are affected by infertility. Importantly, in about half of these cases, male factors serve as contributors. Therefore, if the authors manage to make the printed cells produce sperm, the sperm may potentially be utilized to fertilize an egg through in vitro fertilization (IVF). This can provide a new fertility treatment alternative for couples
Dr. Flannigan's research program—which is a highly collaborative endeavor between researchers across multiple disciplines—has been offering new insights into the molecular and genetic mechanisms that play a contributing role in NOA. Using several single-cell sequencing techniques, the team has gained an understanding of the characteristics and gene expression of every individual cell. The obtained data have been subjected to computational modeling in order to understand the underlying causes of NOA and to find new treatment options.
"Increasingly, we're learning that there are likely many different causes of infertility and that each case is very patient-specific. With that in mind, we're taking a personalized, precision medicine approach – we take cells from a patient, try to understand what abnormalities are unique to them, and then 3D print and support the cells in ways that overcome those original deficiencies," concluded Dr. Flannigan.














