It is nearly impossible to imagine the modern world without antibiotics. Several diseases such as the plague—which once killed people by the millions—are now treatable because of these drugs. Nevertheless, there are concerns surrounding their overprescription. During the COVID-19 pandemic antibiotics such as Azithromycin have been overprescribed. Also, loose regulations facilitate easier availability which enables self-medication. Now, a new study has found that the consumption of antibiotics increases the chances of developing colon cancer.
According to researchers from the Umeå University, Sweden, individuals who took antibiotics for over six months had a 17 percent higher risk of developing cancer in the proximal colon than those who had not been prescribed any. However, no increase in the risk of cancer in the distal colon was found, nor in the risk of rectal cancer in men. In fact, a slight decrease of the latter was noted in women. The authors suggested that the effect of antibiotics on the gut microbiota could be the reason behind the increase.
"The results underline the fact that there are many reasons to be restrictive with antibiotics. While in many cases antibiotic therapy is necessary and saves lives, in the event of less serious ailments that can be expected to heal anyway, caution should be exercised. Above all to prevent bacteria from developing resistance but, as this study shows, also because antibiotics may increase the risk of future colon cancer," said Dr. Sophia Harlid, corresponding author of the study, in a statement.
A Global Concern
Colorectal cancer (CRC) is the third most common cancer in the world. According to the World Health Organization (WHO) over 1.9 million new cases of CRC, and 935,000 deaths due to CRC, were reported in 2020. CRC begins either in the colon (longest section of the large intestine) or the rectum (the lower part of the lowermost part of the large intestine where stool is stored before expulsion).
Age and lifestyle (particularly diet, smoking, alcohol consumption, and lack of exercise, among others) are considered to be the most common factors for CRC. However, conditions such as diabetes, obesity, and inherited syndromes increasing colon cancer risk, are among other factors that can escalate an individual's risk of developing CRC.
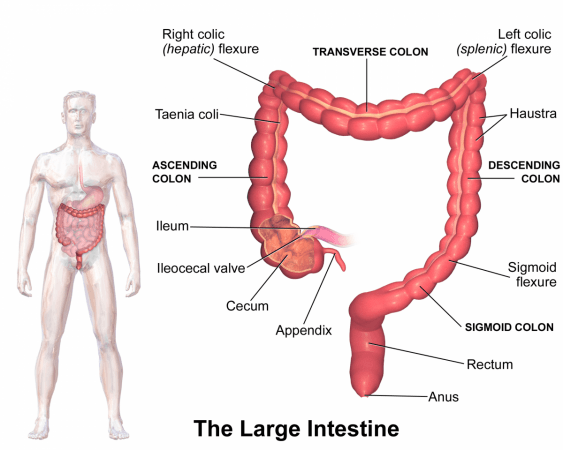
The large intestine can be broadly divided into three main sections. Proximal colon is the first section that includes the beginning and middle parts of the colon. It comprises the caecum, ascending colon, hepatic flexure, transverse colon, and splenic flexure). The second section known as the distal colon is the last section of the colon and is composed of descending colon and the sigmoid colon. Rectum forms that lowest section.
Linking Cancer and Antibiotic Use

For the study, the authors used data of 40,545 patients (men=21,458, women=19,087) from the Swedish Colorectal Cancer Registry who had been diagnosed with CRC between 1 January 2010 and 31 December 2016. Depending on the nature of the cancer, the cases were categorized as proximal colon cancer, distal colon cancer, or rectal cancer. Based on the stage of CRC, the cases were classified as early stage (stage I-II) and late stage (stage III-IV).
Data from a matched control group of 202,720 cancer-free individuals (men=107,285, women=95,435) was chosen from the Swedish population at large and compared to that of the patients with CRC. The sampling was done in a manner (incidence density sampling) that ensured reduced bias while utilizing cases and controls having different follow-up periods. The information about the use of the antibiotics by the individuals was obtained from the Swedish Prescribed Drug Register for the period 2005–2016
Higher Use, Higher Risk

Through their analysis, the team learned that 18.7 percent of all CRC cases, and 22.4 percent of the controls had not been prescribed any antibiotics during the study period. 20.8 percent of CRC cases, and 19.3 percent of controls had consumed antibiotics for over 2 months. Among the CRC patients, 36.5 percent had been diagnosed with proximal colon cancer, 29.3 percent had distal colon cancer, and 33 percent had rectal cancer. The median follow-up duration was 8 years, and the mean age of CRC diagnosis was 72 years.
The scientists noted that there was a visible risk of colon cancer at five to ten years after taking antibiotics itself. As expected, the rise in risk was the highest among those who took antibiotics the most. The increase in the risk of proximal colon cancer was 9 percent for moderate use (10 days to 2 months) of antibiotics, while it was 17 percent for very high use (over six months). However, the strongest increase in the risk of cancer was found to be in the ascending colon (14 percent).
Interestingly, the study did not find any increase in the risk of cancer within the descending colon due to the use of antibiotics. However, an inverse association or decrease in risk of rectal cancer was observed, particularly in women (around 9 percent).
Potential Role of Gut Microbiome

With a strong link established between antibiotic use and elevated cancer risk, the authors sought to understand how antibiotics these risks. Therefore, they investigated a non-antibiotic bactericidal drug, methenamine hippurate, prescribed for the treatment of urinary infections. These drugs do not impact the microbiome. They gleaned that there was no difference in the incidence of colon cancer among those who used the drug. This, according to the authors, indicated that it is the effect of antibiotics on the microbiome that escalates the risk of cancer.
Though the current study analyzed only orally administered antibiotics, it is likely that intravenous antibiotics may also impact the gut microbiota found in the intestinal system. In spite of these findings, it is not possible to overlook the role of antibiotics in treating diseases "There is absolutely no cause for alarm simply because you have taken antibiotics. The increase in risk is moderate and the affect on the absolute risk to the individual is fairly small," assured Dr. Harlid.
Stressing on the importance of regular screening for CRC, Dr. Harlid informed that Sweden—where the study was conducted—is in the process of introducing routine screening for the disease. "Like any other screening programme, it is important to take part so that any cancer can be detected early or even prevented, as cancer precursors can sometimes be removed," she concluded.













