The scientific community has been occupied with the COVID-19 pandemic for nearly two years now. However, another pandemic has raged for decades and continues to persist across the world—human immunodeficiency virus (HIV) infection. While treatments to tackle the condition exist, its eradication has remained impossible. Now, scientists have reported the discovery of the role of a sugar on the surface of HIV-infected cells that aids them in evading the immune system.
Through a new multi-institutional study, researchers discovered that HIV-infected cells utilize a type of sugar molecule called sialic acid to hide from the immune system and evade immune surveillance of natural killer (NK) cells. The authors also demonstrated that disabling the sugar helped NK cells target and kill infected cells specifically.
"We identified a glyco-immune checkpoint interaction as a novel mechanism that allows HIV-infected cells to evade immune surveillance. And we developed a novel approach that selectively targets these interactions on the surface of these infected cells," said Dr. Mohamed Abdel-Mohsen, co-author of the study, in a statement. The findings were published in the journal PLOS Pathogens.
A Global Killer
HIVs are retroviruses that invade and infect cells that are associated with the immune system and protect the body from infections. This can eventually lead to acquired immunodeficiency syndrome (AIDS), where the immune system becomes weak and incapable of defending the body, thereby, leaving it vulnerable to other infections and diseases.
According to the WHO, as of 2020, around 38 million people live with HIV/AIDS worldwide. Approximately 680,000 lost their lives due to HIV-related causes in 2020 alone. It can affect people of any age, and is transmitted through contact with body fluids of infected persons and through sexual contact. It can also spread via other routes such as blood transfusions or from mother to fetus.
Unfortunately, there is no effective cure or treatment for long-term remission of HIV/AIDS. Antiretroviral therapy (ART) is the only existing treatment that has been found to benefit patients with HIV. While it can reduce the amount of the virus in the body, it cannot eliminate the pathogen completely. Lapse or discontinuation of treatment can result in the worsening of a patient's health.
Acting as Inhibitors
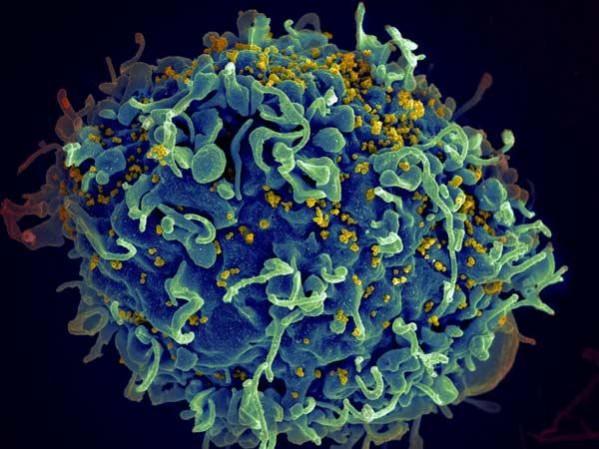
For the study, the authors examined a kind of sugar known as sialic acid that is found on the surface of cells infected with HIV. These sialic acid sugars bind with siglecs (siglec-9 in this case), special receptors found on the surface of natural killer immune cells. Upon activation, these receptors function as inhibitors that restrict killer cells and prevent them from killing infected cells.
Having learnt that this was the case, the team contemplated whether infected cells can make use of this inhibitory mechanism to elude immune surveillance. "We thought, 'is it possible that these HIV-infected cells are using this interaction — covering themselves with these sugars to evade the natural killer immune surveillance?" averred Dr. Abdel-Mohsen.
Disabling A Crucial Sugar
The authors analyzed whether this association could be manipulated to enable killer cells attack and kill HIV-infected cells more efficiently. First, they scrutinized whether the disabling of the inhibitors on the killer cells could help achieve their full killing potential. However, this can result in both healthy and infected cells being indiscriminately attacked and destroyed by the immune cells.
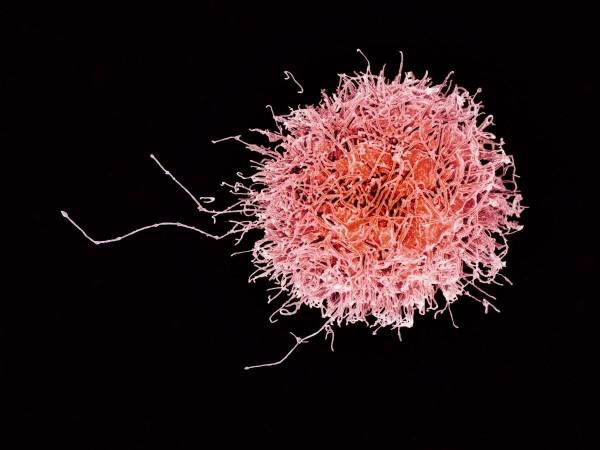
Thus, the scientists took a closer look at the HIV-infected cells themselves. Using an enzyme known as sialidase, they removed sialic acid sugars that were responsible for the activation of the immune inhibitors. Nevertheless, all cells were found to be affected as the killer cells indiscriminately targeted and attacked cells.
Finally, the researchers created a sialidase conjugate attached to HIV antibodies. Amazingly, the antibody-sialidase conjugate was found to target only sialic acid present on HIV cells. With the removal of sialic acid from these cells, the killer immune cells were able to attack and kill only HIV-infected cells, thereby, leaving healthy cells unaffected.
Dr. Abdel-Mohsen expressed, "The killer cells become a super killer for the HIV-infected cells and they now attack them in a selective manner. The discovery could be a missing link in the 'shock and kill' approach to HIV treatment that has been a focus of research for the past several years.
Scope for Broad Application
The 'shock and kill' approach is a two-step process. It involves 'shocking' HIV out of latency first in order to ensure that it is detectable. Next, the immune system is stimulated to 'kill' the pathogen completely. Unfortunately, despite the discovery of effective methods to reverse latency, an efficient way to improve the killability of HIV-infected cells after reactivation remains elusive.
"We may have the shock, but we don't have yet the kill. Our method actually increases the susceptibility of HIV-infected cells to killing, which is one of the top unmet needs in the HIV field," explained Dr. Abdel-Mohsen.
Dr. Samson Adeniji, first author of the study, stated that the approach described by the team could be evaluated in combination with other neutralizing antibody treatments that are currently in clinical trials. "By combining approaches, we could turn these immune cells from a cop into a kind of Robocop," he stressed. The authors also highlighted that other infectious diseases such as COVID and hepatitis—that also dodge the immune system—can serve as candidates for the approach's clinical application.
The next step for the team is to conduct animal studies for the in vivo testing of the findings. Also, they aim to investigate other molecules on HIV cells to ascertain whether they play roles similar to sialic acid. "HIV-infected cells are likely evading immune surveillance through many potential glyco-immune checkpoints. We are investigating other mechanisms and how to break them," concluded Dr.Abdel-Mohsen.














