While the lungs are the primary target of the SARS-CoV-2 coronavirus, other organs of the body can also bear the brunt of the disease. Several individuals who contract COVID-19 have been found to suffer damage to the kidneys—Acute kidney injury (AKI). Nevertheless, it is not certain whether the virus plays a direct or an indirect role in this. Now, scientists have found that despite being able to infect human kidney cells, the coronavirus may not typically cause cell death within the organ.
According to a new study by a team of Israeli researchers, the SARS-CoV-2 virus can infect and replicate within human kidney cells. However, it may not result in the kind of cell death that is found in organs such as the lungs. The authors also found that kidney cells that already exhibit signs of injury may be more easily invaded by the pathogen and can develop additional injuries.
"SARS-CoV-2 can infect kidney cells without a cytopathic effect. AKI-induced cellular proliferation may potentially intensify infectivity and tubular damage by SARS-CoV-2, suggesting that early intervention in AKI is warranted to help minimize kidney infection," the authors wrote.
Extensive Renal Damage Among COVID-19 Patients
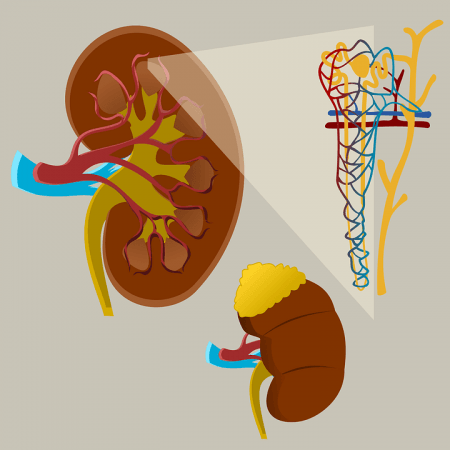
AKI is a widespread complication among hospitalized COVID-19 patients. Studies have noted that the incidence rate of AKI among such patients can be anywhere between 39 to 52 percent. Mortality rates among COVID-19 patients have also been found to be driven higher due to severe renal damage, with some studies finding that only 30 percent survive. Therefore, understanding the role of the SARS-CoV-2 in AKI is of paramount importance.
In order to investigate the level of the novel coronavirus' involvement in kidney injury, the team cultivated human kidney cells in the lab and infected them with the virus. The cells used in the experiments were cultured as three-dimensional spheroids—enabling the imitation of a healthy kidney—or as a two-dimensional layer that mimicked the cells of a severely injured kidney.
The spheroids were examined for the expression receptors ACE2 (angiotensin-converting enzyme 2), BSG/CD147 (Basigin/ cluster of differentiation 147) and TMPRSS2 (Transmembrane serine protease 2)—the cellular proteins, particularly ACE2, that the SARS-CoV-2 uses to gain entry into cells. Significantly higher levels of the receptors were found to be expressed by the three-dimensional cells in comparison to 2D cell layers, thereby, providing ideal conditions for the virus to infect cells.
Hurting Without Killing
The authors found that in spite of entering, infecting, and replicating within human adult kidney cells, the novel coronavirus did not typically cause cell death. Before being infected, the cells contained high levels of type 1 interferon(IFN)-related molecules —cytokines or signaling proteins that are produced by cells as a response to infections. When the cells were infected, the infection was found to trigger an inflammatory response that led to the increase of IFN-related molecules.
However, kidney cells that possessed inadequate amounts of the cytokine molecules died upon being infected. This suggested that the stimulation of inflammatory response of the signaling chemicals provided a protective effect. The study also gleaned that cells that imitated a severely injured kidney had higher susceptibility to infection and further injury, but not cellular death.
"The data indicate that it is unlikely that the virus is a primary cause of acute kidney injury seen in COVID-19 patients. It implies that if such injury takes place in the kidney by any cause, the virus might jump on the wagon to intensify it. Therefore, if we're able to limit the common scenario of acute kidney injury in the first place, then there might be the possibility to minimize potential damage caused by the virus," illustrated Dr. Benjamin Dekel, lead author of the study, in a statement.












