Without chemotherapy, the management of cancer is unimaginable. It has given countless sufferers a chance to fight the disease and keep it at bay, extend their lives, and return to relatively normal health. However, what if the very treatment that helps you beat the disease can make it come back? A new study has reported that a group of chemotherapy drugs can result in mutations that may trigger the relapse of blood cancer in children.
According to a study spanning across three countries, chemotherapy drugs known as thiopurines can induce mutations that can lead to the relapse of acute lymphoblastic leukemia (ALL)—a form of blood cancer—in children and adolescents. The study provides the very first direct experimental and genomic evidence of drug resistance mutations induced by chemotherapy in pediatric cancer patients.
"The findings offer a paradigm shift in understanding how drug resistance develops. The results also suggest possible treatment strategies for ALL patients who relapse, including screening to identify those who should avoid additional thiopurine treatment," said Dr. Jinghui Zhang, co-corresponding author of the study, in a statement.
Dominant Cancer Among Children

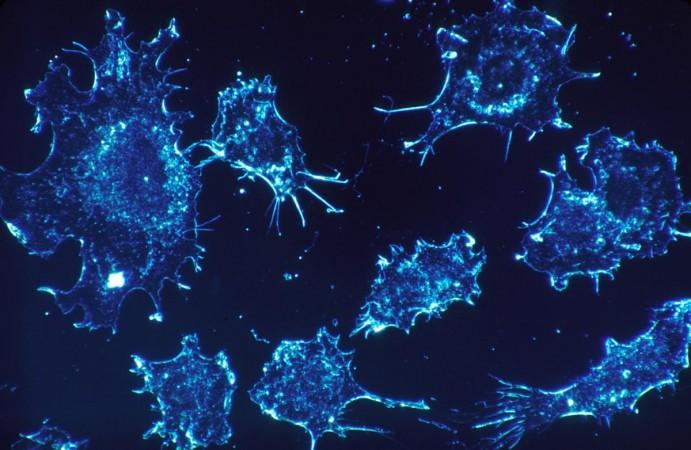
Acute lymphoblastic leukemia (ALL) begins in white blood cells with the bone marrow. Errors developed in the DNA of the bone marrow cells lead to the excessive production of lymphocytes, thereby, resulting in its occurrence. It is highly progressive and can affect other blood cells such as red blood cells, platelets, and white blood cells. It is also the most common childhood cancer.
Thiopurines are immunosuppressants that are used for the treatment of autoimmune disorders and organ transplant recipients. They are also prescribed for the treatment of inflammation. In the case of ALL, thiopurines are used for chemotherapy. According to the WHO, 80 percent of ALL cases occur in children. Relapse is the main cause of death in children and adolescents with ALL across the world.
Mutations Induced By Chemotherapy
For the study, the team collected samples from pediatric patients—in whom ALL had relapsed—in China, Germany, and the US. Over 1,000 samples obtained from patients at different points during their treatment were examined by the authors. This included samples collected from 181 patients at diagnosis, remission, and relapse. Through their analysis, the scientists discovered a mutational signature that enabled the decoding of the mechanism.

Mutational signatures are the patterns of somatic mutations (change in the DNA sequence of somatic cells) that are hidden in cancer genomes. They represent the history or timeline of genetic alterations in cells. The scientists connected escalated thiopurine-induced mutations to gene such as the MSH2 that undergo mutations in leukemia. MSH2 gives instructions for production of a protein that plays a crucial role in the process of DNA repair.
It was found that the mutations lead to the inactivation of a DNA repair process known as mismatch repair. This caused ALL to become resistant to thiopurines. This combination led to a 10-fold increase in ALL mutations, which included a variation in the gene TP53 that suppresses tumors. Alarmingly, the mutation, TP53 R248Q, triggered resistance to other chemotherapy drugs such as cytarabine, daunorubicin, and vincristine.
DNA Errors and Drug Resistance
Using two cell lines in the lab, the team reproduced the thiopurine-induced TP53 mutations and resistance to chemotherapy. "This study not only changes our ALL treatment considerations, but also opens the door to study mechanistically how defective repair generates drug-resistant mutations," highlighted Dr. Zhou.
According to the researchers, treatment-induced mutations are involved in an estimated 25 percent of pediatric ALL relapse. Even in the current study, eight percent of patients showed evidence of thiopurine-associated mismatch-repair signature.
Dr. Zhang averred, "In the future, it may be possible to monitor bone marrow during treatment as a way to detect these mutational signatures early enough to help identify at-risk patients who may be candidates for emerging therapies like CAR-T cells." However, the authors emphasized that most patients who receive thiopurine treatment are not affected by the thiopurine-induced mutations, and the benefits exceed the risks.








