Resistance to several life-saving drugs has emerged as a concerning global health challenge. As pathogens become resistant to medications, fears surrounding the resurfacing of diseases—that have been rendered largely manageable—as major threats are on the rise; particularly in underdeveloped and developing nations. Now, a new study has stated that malaria parasites in Africa have developed resistance to a crucial family of front-line malaria drugs.
According to an international study, Plasmodium falciparum, the pathogen behind most of Africa's malaria cases, has developed resistance against the drug artemisinin and its derivates. The researchers also identified two mutations, A675V and C469Y, in P. falciparum that were found to have a correlation with longer durations required for clearance of the parasite. The findings were published in the New England Journal of Medicine.
"The association that we found between clinical artemisinin resistance and the presence of the A675V and C469Y mutations raises the possibility that these resistance markers can be used to assist in the detection of artemisinin resistance among patients with P. falciparum infection in Africa," wrote the authors.
A Deadly Disease

Malaria is caused in human beings by five parasitic protozoa from the Plasmodium family. They are transmitted through the bites of infected female Anopheles mosquitoes that are the primary vectors. Two of these protozoans—Plasmodium falciparum and Plasmodium vivax—pose the biggest threats. Malaria causes several complications including damage to organs such as the kidneys and the liver, and can also result in the rupturing of the spleen.
According to the WHO, P. falciparum was responsible for 50 percent of infections in South-East Asia, 65 percent in the Western Pacific regions, 71 percent in the Eastern Mediterranean, and 99.7 percent of cases in Africa. P. vivax led to 70 percent of the malarial infections in the Americas. Children accounted for nearly 67 percent of all Malaria deaths worldwide in 2018. P. falciparum and P. vivax are associated with over 400,000 deaths every year.
Edge Over Other Drugs
The 'gold standard' for treating malaria caused by P. falciparum is the use of a family of drugs comprising artemisinin and its derivates. Artemisinin is obtained from the extract of sweet wormwood (Artemisia annua), a herb used in traditional Chinese medicine. It was discovered in 1972 by Dr. Tu Youyou, for which she was awarded the Nobel Prize in Physiology or Medicine in 2015. Nowadays, therapies aimed at treating malaria caused by the other members of the Plasmodium group also involve the standard administration of artemisinin.
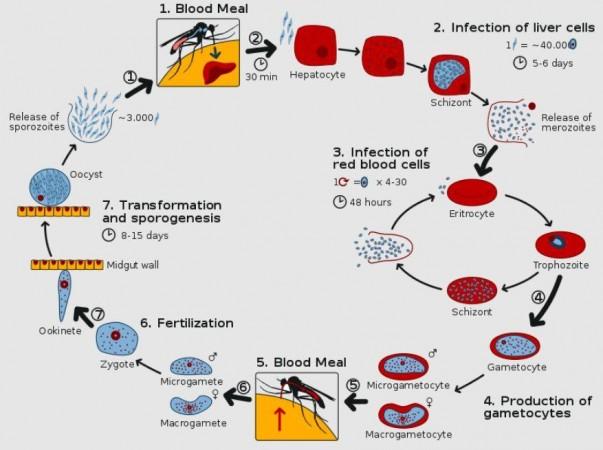
The life cycle of malaria parasites is complex. It is characterized by several rounds of asexual replication in various stages and tissues—both in the intermediate vertebrate host and in the insect host. Within human beings, the Plasmodium life cycle involves two types of cells: hepatocytes (liver tissues) and erythrocytes (red blood cells, or RBCs). The biggest advantage that artemisinin and its derivatives have over other drugs in the treatment of malaria is that they can rapidly kill all the parasite's life cycles.
Evaluating Drug Resistance
For the study, the authors analyzed data from malaria patients—infected with P.falciparum—at St. Mary's Hospital Lacor in Gulu, Uganda, between 2015 to 2019. They examined the effect of artesunate (an artemisinin drug) on 240 patients who were treated with it. These individuals were administered three doses of the drug within 24 hours.
Blood samples were regularly collected from the patients and examined for traces of the pathogen. In order to signify in vivo artemisinin resistance, the team evaluated a clearance half-life longer than five hours (i.e) survival of the number of parasites five hours following the initial dose of the drug. This meets the definition of resistance set by the WHO.

In most of the cases, the protozoan was cleared quickly. However, 5.8 percent of the cases (14 participants) exhibited artemisinin resistance. Over half the number of parasites were found to still survive five hours post the first dose of the medicine. The percentage of patients displaying this resistance remained steady between 2017 and 2019.
Resistance-inducing Mutations
In addition to observing in vivo artemisinin resistance in the patients, the authors also examined the genotype of the parasitic protozoan that the patients were infected with. The authors identified seven mutations in a gene called kelch13 in the P.falciparum, among 15.8 percent (38 patients) of the cases. Of these mutations, two concerning ones—labeled A675V and C469Y—were the most prevalent.
While the mutations had already been noted in malaria parasites in the continent, their resistance to medications was not certain. "We didn't know if these parasites were actually resistant to drugs in humans," said Dr. Toshihiro Mita, co-author of the study, according to Nature. A675V and C469Y mutations have been linked to antimalarial resistance in southeast Asia.

It was also found that the two genetic alterations had a correlation with a longer clearance half-life. According to the scientists, they can be utilized as predictive markers for resistance to the anti-malarial drug. As of now, the WHO has classified A675V and C469Y as candidate markers. Based on the findings of the current study, updating the mutations, particularly A675V, to proper molecular resistance markers seems an immediate necessity.
Independent Emergence of Mutations
Through the comparison of the Asian and African A675V mutants, the researchers revealed that they had different origins (i.e) resistance to artemisinin originated separately in Africa, and not as a consequence of parasitic immigration. The authors suggested that the uncontrolled use of injectable artesunate could be a potential reason for the emergence of drug-resistant mutants.
Previous studies have also shown an association between the presence of mutations and resistance to artemisinin. The results of the current study, adds to the growing evidence that calls for re-evaluation and formulation of therapies to address this antimalarial resistance. The authors warned that it, "Poses a potential risk of cross-border spread across Africa, highlighting the need to perform large-scale surveys."

















