It is a known fact that the severity of the disease varies among individuals with COVID-19. While some experience asymptomatic infection of the SARS-CoV-2 virus, others succumb to it. The crucial factor in the varying outcomes among patients is the differing immune responses. Now, scientists have discovered the underlying metabolic changes that regulate the manner in which immune cells and plasma respond to the disease.
According to a multi-institutional study, that scrutinized blood samples from nearly 200 patients, these metabolic changes are associated with the severity of the disease. The research investigated metabolic changes in plasma and immune cells, and suggested that their variations in different patients can be utilized to predict patient survival.
"We analyzed thousands of biological markers linked to metabolic pathways that underlie the immune system and found some clues as to what immune-metabolic changes may be pivotal in severe disease," said Jihoon Lee, co-first author of the study, in a statement. The findings were published in the journal Nature Biotechnology.
Analysing Plasma and Immune Cells
The diversity of immune reactions among different COVID-19 patients has been identified as a differentiating factor in the outcome. While some suffer a simple flu-like bout, others require hospitalization and ventilator assistance. "We know that there are a range of immune responses to COVID-19, and the biological processes underlying those responses are not well understood," noted Lee.
Also, much of the data studied is done in isolation; often providing an incomplete picture. Talking about the technological challenges that the current paper addressed, Dr. Jim Heath, co-corresponding author of the study, said, "Many of the data sets that are collected from these patients tend to measure very different aspects of the disease, and are analyzed in isolation. Of course, one would like these different views to contribute to an overall picture of the patient."
For the study, the authors collected 374 blood samples from 198 individuals with varying severities of COVID-19. In order to ascertain the course of the acuteness of illness in individual patients, the samples were collected at clinical diagnosis and several days later when they continued to be symptomatic in the acute phase.
The team studied plasma and single immune cells in the samples, and their evaluation included 1,387 genes that are involved in metabolic pathways (excluding classical immune markers) and 1,050 plasma metabolites.
Changes In Metabolites
Through their examination of the plasma samples, the scientists learnt that metabolite alterations were associated with elevated COVID-19 severity. For example, certain metabolites such as phenylalanine and mannose—both of which are considered mortality risk markers—were found to be positively correlated to the severity of the infection.
Adding weight to the role of glycolytic/gluconeogenic processes and anaerobic metabolism in COVID-19, glucose was also observed to be positively associated with disease severity. Also positively correlated were lipids such as linoleic acid that are linked to inflammation. "Thus, increased COVID-19 severity is associated with metabolite alterations, suggesting increased immune-related activity," wrote the authors.
One of the other tests employed was the principal component analysis (PCA) on plasma metabolite levels. PCA is a technique employed for reducing the dimensionality of datasets which increases their interpretability yet minimizes data loss. Using PCA the team aimed to ascertain whether disease severity between individuals could be distinguished through plasma metabolite levels.

A clear difference was found between individuals with mild COVID-19 and those who had more severe forms. Metabolites such as linoleic acid-containing glycerophospholipids and sphingomyelins served as the main contributors to the severity of the disease. "Taken together, COVID-19 severity is associated with many changes in plasma metabolite levels, which can be ascribed to distinct metabolic pathways that potentially impact immune responses," the study said.
Metabolic Changes in Immune Cells
Along with changes in the plasma, several immune cells were also observed to undergo metabolic changes. It was noted that CD8+ T cells (or T-killer cells) formed a small yet metabolically hyperactive subpopulation of immune cells—presumably SARS-CoV-2 specific—exhibited rising metabolic activity as the severity of the disease increased. T-killers cells are lymphocytes that kill cancer cells and cells infected with pathogens such as viruses and bacteria.
Importantly, CD4+ T cells (or T-helper cells) also showed a similar trend as CD8+ T cells where small subpopulations became metabolically ascendant(with elevated activity) with the severity of COVID-19. However, the authors noted that "Different subpopulations of CD4+ T cells exhibit divergent metabolic activities with increasing disease severity, an observation missed by bulk analyses."
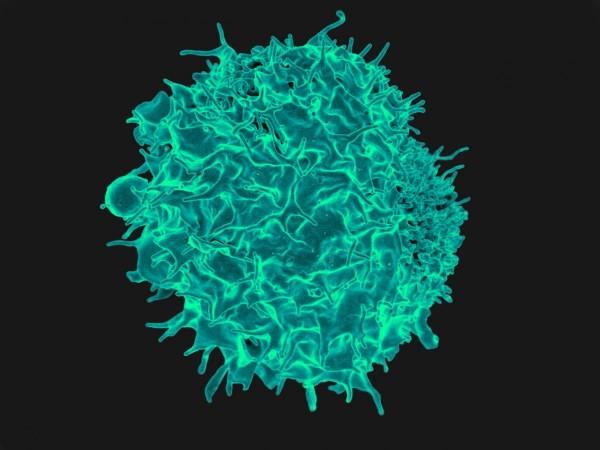
Another finding was that B cells, which is a part of the adaptive immune system, showed increased metabolism in comparison to non B cells. This included a positive correlation of amino acid metabolic activity with the severity of the infection; possibly illustrating the antibody-secreting functional demands in the case of acute disease.
Among other cells that showed metabolic changes were monocytes. It was gleaned that monocytes in COVID-19 patients differentiated into two functionally and metabolically diverse groups—a subpopulation that was inflammatory and metabolically activated, and a non-classical subpopulation that was potentially immunomodulatory and metabolically repressed.
Potential to Predict Outcomes in Patients

Additionally, single-sequencing revealed that every significant immune cell type possessed a distinct metabolic signature. According to the researchers, the metabolic changes in plasma and immune cells may help in predicting patient survival.
"We have found metabolic reprogramming that is highly specific to individual immune cell classes and even cell subtypes, and the complex metabolic reprogramming of the immune system is associated with the plasma global metabolome and are predictive of disease severity and even patient death," said Dr. Yapeng Su, co-first and co-corresponding author of the study.
Dr. Heath highlighted that the process employed in the current research helps in obtaining a better understanding of the novel coronavirus infection. "The approach described here allows for the sum of the different data sets to be much greater than the parts, and provides for a much richer interpretation of the disease," he concluded.








