The medical advancements made in the past few decades have provided cancer patients with a fighting chance at life. Several treatments have helped sufferers of different forms of cancer not to just manage the disease but also to achieve remission.
Immunotherapy is one such remedy. However, the body's resistance to the treatment often serves as a challenge. Now, scientists have developed a new lipid nanoparticle that can deliver immunity-triggering molecules into immune cells in order to overcome this resistance.
A team of Japanese researchers has designed a lipid nanoparticle that can carry immune-signaling molecules into macrophages in the liver to repress resistance to anti-tumor immunotherapy. In an animal study, the lipid known as YSK12-C4 was found to deliver specific signaling molecules to the liver macrophages. The authors found that when combined with a therapy that helped arm cells known as natural killer (NK) cells, resistance was counter-acted.
"The findings suggest that our lipid nanoparticles carrying immune-signaling molecules convert the immune status from immunologically cold to immunologically hot," said Dr. Takashi Nakamura, co-author of the study, in a statement. The findings of the research were published in the Journal for Immunotherapy of Cancer.
Resistance to Treatment
Immunotherapy is a cancer treatment where a patient's own immune system is used to fight the disease. It employs substances produced within the body or those synthesized in a laboratory to enhance the manner in which an individual's immune system functions to locate and kill cancer cells. Cancers such as bladder cancer, childhood cancer, head and neck cancer, leukemia, and advanced lung cancer, among others, are treated using immunotherapy.
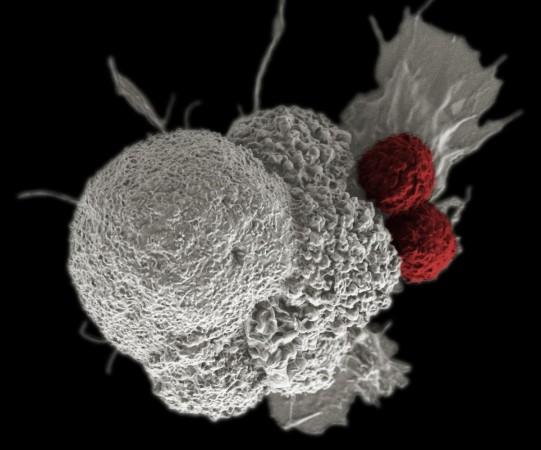
In the treatment, the initialization of checkpoint proteins on the surface of immune cells known as T cells helps moderate their immune response to stop them from attacking other cells in the body indiscriminately. However, certain cancer cells can hijack this mechanism, which in turn prevents immune actions towards them as well. While scientists have formulated immune checkpoint inhibitors that can counter this, several patients remain resistant to these therapies.
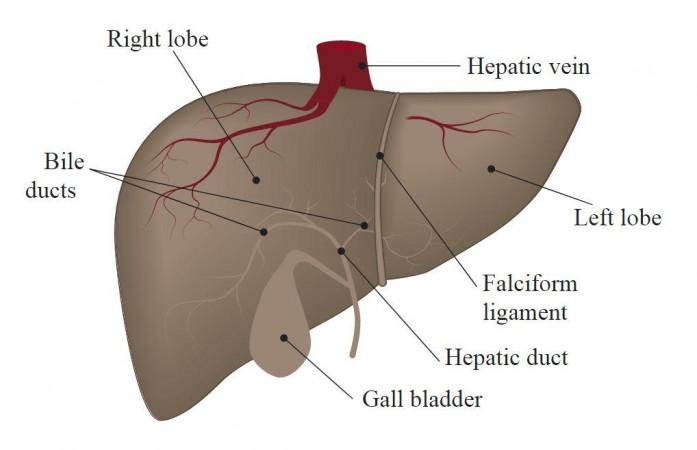
The human liver's role is not confined to metabolic functions and detoxification alone. It is where intricate immunological functions moderated by different immune cells and non-hematopoietic cell groups take place. The body's largest organ is also responsible for the production of cytokines and chemokines, complement components, and acute-phase proteins. Varied populations of immune cells such as macrophages, NK (natural killer) cells, and NKT (Natural Killer T cells), are also present in the liver.
Being the most abundant immune cell in the liver, these specific macrophages are also known as Kupffer cells. In the current study, the authors designed a novel lipid nanoparticle that could help successfully carry immunity-inducing compounds to these cells in the liver in order to tackle immunotherapy resistance.
Overcoming Suppression of Immune Responses

Called YSK12-C4, the lipid possesses a high affinity towards immune cells. Mice with metastatic melanoma were injected with the nanoparticle intravenously. It was able to carry signaling molecules known as cyclic dinucleotides across the cell membranes of liver macrophages. This triggered the production of immune-related signaling proteins known as type 1 interferons through a stimulator of an interferon gene (STING) pathway.
The produced proteins in turn were released into the bloodstream, which activated NK cells in the lung and spleen. This produced Interferon-gamma (IFNγ), a cytokine (another signaling protein) within the lung metastases. However, independently, this treatment induced a very mild or little anti-tumor effect. This was because the expression of a protein called PD-L1 (Programmed death-ligand 1) on the cancer cells was triggered by IFNγ and type 1 interferon.
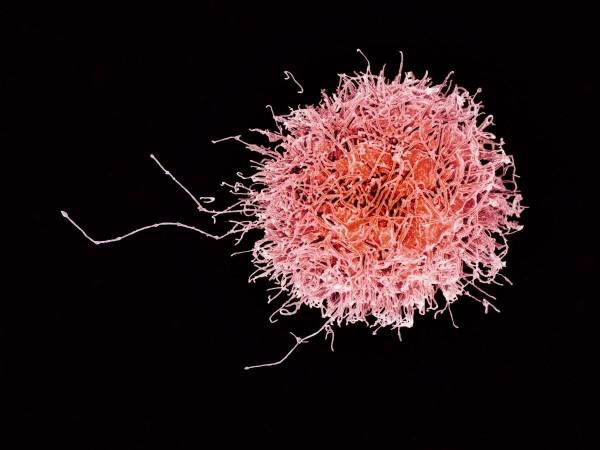
PD-L1 plays a crucial role in the suppression of the adaptive immune system. It hinders the initiation of robust tumor-killing immune response of NK cells that express another important protein known as PD-1 (Programmed cell death protein 1). However, the team found a way to address this. They learnt that by administering an anti-PD-1 immunotherapy treatment, the cancer cells were unable to turn off NK cells.
The NK cells in turn became armed and were able to attack cancer cells. "This could lead to the development of a promising adjuvant that reduces resistance to anti-PD-1 antibody treatment in some cancer patients," expressed Dr. Nakamura. Nevertheless, the scientists noted that additional research will be required to ascertain if this treatment can lead to liver toxicity and whether other signaling molecules can be utilized.
Resistance to Cancer Immunotherapy








!['Lip lock, pressure, pyaar': Vidya Balan- Pratik Gandhi shine in non-judgmental infidelity romcom Do Aur Do Pyaar [ Review]](https://data1.ibtimes.co.in/en/full/797104/lip-lock-pressure-pyaar-vidya-balan-pratik-gandhi-shine-non-judgmental-infidelity-romcom.jpg?w=220&h=138)








