A new study has recently revealed that tiny robots might help in targeting tumors and destroying them. Researchers at Arizona State University (ASU) in collaboration with those from the National Center for Nanoscience and Technology (NCNST), of the Chinese Academy of Sciences, successfully programmed the technology that can shrink tumors by cutting off their blood supply.
Dr Hao Yan of Arizona State University said in a press release: "We have developed the first fully autonomous DNA robotic system for a very precise drug design and targeted cancer therapy."
However, the nanorobots are not exactly like how they sound. They are called "robots" because they are programmed to do specific and unique tasks. They are made out of organic materials and in this case, it's DNA.
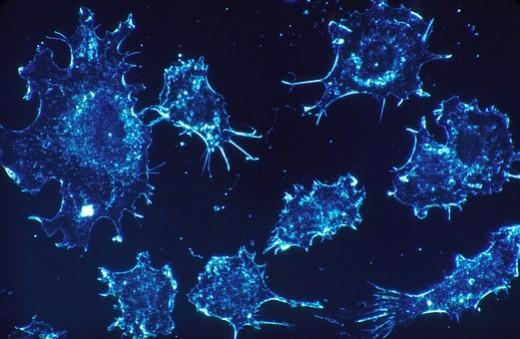
Cancer treatment is challenging, the reason being it becomes difficult to just destroy the tumor without damaging the healthy cells.
Chemotherapy and radiation treatments also effectively shrink many kinds of tumors, but both forms of treatment hit healthy cells as well. They can also cause severe side effects and weaken the immune system.
This is where nanorobots come to the rescue. They can seek and destroy cancerous tumors, while not harming any healthy cells.
In the Arizona State University (ASU) study, scientists injected human cancer cells into a mouse to induce aggressive tumor growth. Once the tumor was growing, the nanorobots — which are a thousand times smaller than a strand of human hair — were deployed.
Each of the nanorobots is made from a rectangular flat DNA origami sheet with the blood-clotting enzyme thrombin attached to their molecular guiding system.
The blood-clotting enzyme has the capability of blocking tumor blood flow by clotting the blood within the vessels that feed it. Scientists explain it by saying that it causes a sort of mini heart attack, leading to the death of the tumor tissue.
The researchers hope that now that their method has proved effective and safe in mice, it might soon help in cancer treatment in humans.








